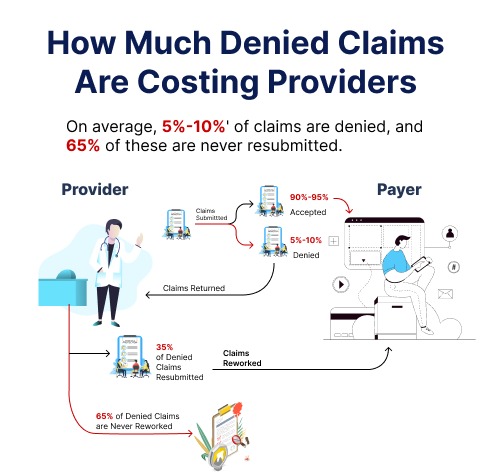
Payment denials cost the majority of healthcare organizations between 6 and 8 percent of their total income. Healthcare providers cannot afford to overlook a loss of this size because these payment refusals have an immediate effect on their sources of income. Effective denial management services play a crucial role in this regard.
Effectively handling payment rejections is essential to increasing sales and gaining the loyalty of your clients. According to a renowned advisory group, 90% of claim denials are completely preventable. They still arise often though.
Denials of medical claims can be very frustrating. It can be very expensive in terms of time, money, and effort for medical practices. Even errors and improperly submitted claims may result in penalties and fines that could drive up your costs.
Here are 10 steps to implement effective denial management services in healthcare:
- Recognize the reasons behind the claims’ denial:
Understanding the reasons for the denial of your patient’s claims is an essential first step. By being aware of these potential problems, you may streamline your processes to optimize your revenue and prevent claim denials. Assisting patients with their insurance claims guarantees a solid, enduring rapport with them. The prompt assistance that you give your patients greatly contributes to the success of your business. Thus, to guarantee the efficient operation of hospital responsibilities, comprehend the causes of claims denial and explain them to your patients.
2. Streamline the process of denial management:
Are you correcting your inaccurate claims manually? We agree that it’s a feasible temporary measure. On the other hand, taking a broader view, you might want to think about using a more efficient procedure. An efficient process offers an ongoing solution and helps you minimize similar problems in the future. Your credibility and income are at risk if you fail to maintain track of rejected claims and have incomplete records. Reduce the workload of your employees by tracking and managing denied claims using a well-organized system. More recent products on the market facilitate effective denial handling and monitoring for your staff. So, when resolving recurrent problems, consider the whole picture.
3. Compute Claims in One Week:
65 percent of claims that are denied are never submitted again. It’s essential to have a proactive claims management staff to prevent these problems from getting worse. Your employees ought to be proficient in handling claims and resubmitting any appeals upon request. Establishing a solid denial strategy is aided by developing a robust workflow to handle the claims denial processes. Once an insurance carrier denies a claim, your team needs to move quickly to file the claim and get it processed within a week. Your payment will be processed quickly with the help of an active claims team. If there are any frequent mistakes that keep happening, think about enhancing your claims filing approach to deal with such problems.
4. Establish a Record for Claims Denials
With claims denial log, all pertinent information may be kept up to date. An even better option is an electronic version of the log, which guarantees that pertinent data is accessible to everyone in the company. To evaluate and improve upon your claim denials, you can review and store correspondence and records from many insurance companies. Furthermore, you will be able to document the dates of services, the requested sum, the unique claim numbers, and the rejected medical codes for convenient access in the future. Establishing a claim record enables you to evaluate previous filing errors and make improvements for an improved coding and billing system. Furthermore, you save one minute on each transaction when you use electronic payments. So, to process claims, keep a record of your correspondence with the insurance companies.
5. Determine Typical Patterns in Healthcare Claims Denials
The healthcare sector is evolving at a rapid pace, just like all other industries. The claims denial industry’s trends are always evolving to stay up with the changing healthcare landscape. An automated denial management procedure is established by identifying the several typical forms of denials. You can have a better understanding of the main problems your claims denial management team encounters by analyzing these trends. Upgrades to the applications that fix these problems thus regularly save you money. Therefore, increase your understanding of these patterns to gain a competitive advantage and make significant financial savings.
Conduct a thorough analysis of denied claims to identify patterns and common reasons for denials. Categorize denials based on factors such as payer, type of denial, and frequency. Determine recurring patterns in denials and put preventative measures in place to avoid them in the future. Update policies and procedures on a regular basis to conform to evolving payer requirements.
6. Outsource your denial management process
Consider about hiring an experienced medical billing company to deal with your denial management issues. Effective outsourcing allows you to receive quick claims processing while saving time and resources.
Skilled denial management companies manage all of the insurance system’s complexities on your behalf. You can focus on your main expertise by assigning these responsibilities to a capable organization. Therefore, outsource to trustworthy businesses your substantial denial management challenges to save time, effort, and money.
7. Use Technology:
Use revenue cycle management solutions and advanced billing applications to assist identify possible problems before claims are filed. Utilize technology to decrease inaccuracies and expedite coding procedures. Design a streamlined and efficient workflow for claims submission, including a clear process for handling denials. Minimize manual entry and reduce the chances of data entry errors.
8. Frequent Training Sessions:
Make sure that staff responsible for billing and coding receive regular training on the most recent billing and coding requirements. Organize frequent training sessions to address typical mistakes that result in denials. If you hire a medical billing company, they will manage all your medical billing and coding requirements and provide frequent training sessions to their staff to prevent denial management. Therefore, it is suggested to hire a medical billing company for efficient denial management solution.
9. Monitor Key Performance Indicators (KPIs):
Create and keep track of key performance indicators (KPIs) for denial management, such as the denial rate, days that accounts receivable (AR) are outstanding, and the resolution time. Analyze data to track performance and pinpoint areas in need of improvement.
Provide a well-organized appeal process for rejected claims, with deadlines for filing. Make sure that employees are knowledgeable about the requirements for various payers and the appeals process.
10. Collaboration with Payers:
Maintain open channels of contact in order to quickly resolve denials with payers. Hold frequent meetings with payer representatives to discuss problems and optimize procedures.
Healthcare businesses can increase overall financial performance, lower revenue loss, and reinforce their denial management services by putting these strategies into practice. Hire a reputable medical billing company to get efficient denial management services while saving your time and energy to see more patients.
